Uterine arterio venous malformations or AVM are a known complication of medical procedures including MTP or medical termination of pregnancy.
This is one such case.
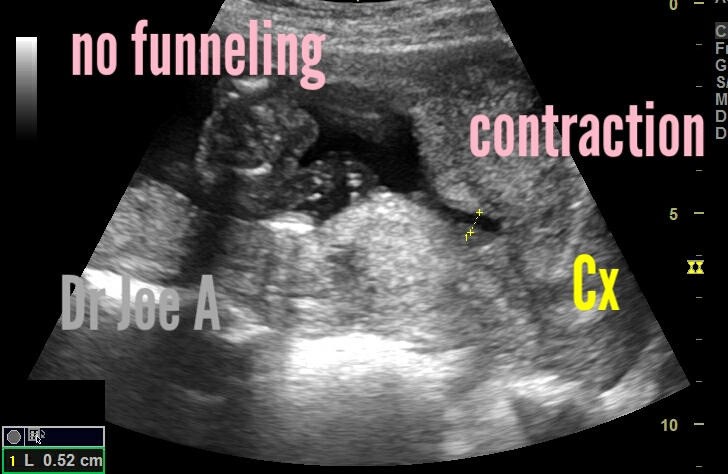
Ultrasound images are shown below:
Ultrasound imaging and color Doppler and spectral Doppler ultrasound findings in this case:
Greyscale ultrasound:
* Well-defined, vascular lesion with a characteristic "honeycomb" appearance.
* The lesion is located in the posterior wall of the uterus, but it can also be found in other areas of the uterus.
* The lesion may be small or large, and it may be single or multiple.
Color Doppler ultrasound:
* The lesion shows intense vascularity with multiple tortuous vessels.
* There is often high-velocity, low-resistance blood flow within the lesion.
* The blood flow may be turbulent, and there may be areas of reversed flow.
Spectral Doppler ultrasound:
* The spectral Doppler waveform shows high peak systolic velocity (PSV) and low resistive index (RI).
* The waveform may be biphasic or monophasic.
* There may be areas of reversed flow.
These findings are not specific for uterine AVM, and they can be seen with other conditions, such as leiomyoma, adenomyosis, and endometrial hyperplasia. However, the combination of these findings is highly suggestive of uterine AVM.
In addition to ultrasound, other imaging studies that can be used to diagnose uterine AVM include:
*Computed tomography (CT) angiography:
* This is a more detailed imaging study that can provide information about the size, location, and extent of the lesion.
* Magnetic resonance imaging (MRI) angiography:
* This is another detailed imaging study that can provide information about the size, location, and extent of the lesion.
The differential diagnoses for uterine AVM on ultrasound include:
*Retained products of conception (RPOC): This is when tissue from a pregnancy remains in the uterus after a miscarriage or abortion. It can cause a hypervascular mass on ultrasound.
* Gestational trophoblastic disease (GTD): This is a group of diseases that can develop after a pregnancy. It can cause a hypervascular mass on ultrasound.
*Hemangioma: This is a benign tumor made of blood vessels. It can cause a hypervascular mass on ultrasound.
* Postpartum uterine pseudoaneurysm: This is a blood clot that forms in an artery in the uterus after childbirth. It can cause a hypervascular mass on ultrasound.
*Subinvolution of the placental bed: This is a condition where the placenta does not completely detach from the uterus after childbirth. It can cause a hypervascular mass on ultrasound.
It is important to distinguish between uterine AVM and these other conditions, as the treatment for each condition is different. Color Doppler ultrasound can be used to help make the diagnosis.
Key features that can help distinguish between uterine AVM and the other conditions:
*Uterine AVM typically has a complex appearance with multiple vessels, while RPOC, GTD, hemangioma, postpartum uterine pseudoaneurysm, and subinvolution of the placental bed are more likely to have a simple appearance with a single vessel.
Images in this case are courtesy of Ms. Regina Rachael.
* Uterine AVM typically has high-velocity flow, while RPOC, GTD, hemangioma, postpartum uterine pseudoaneurysm, and subinvolution of the placental bed are more likely to have low-velocity flow.
* Uterine AVM is often associated with a history of uterine trauma, while RPOC, GTD, hemangioma, postpartum uterine pseudoaneurysm, and subinvolution of the placental bed are not typically associated with a history of uterine trauma.
Management and prognosis:
The management of uterine AVM depends on the severity of the bleeding and the patient's desire for future fertility. In some cases, expectant management may be appropriate. This involves monitoring the patient's bleeding and treating any symptoms that occur.
In other cases, more aggressive treatment may be necessary. This may include uterine artery embolization, hysterectomy, or medical therapy.
Uterine artery embolization is a minimally invasive procedure that involves injecting small particles into the uterine arteries to block the blood flow to the AVM. This can be a very effective treatment for uterine AVM and can help to reduce or stop the bleeding.
Hysterectomy is the surgical removal of the uterus. This is a more drastic treatment option, but it may be necessary in cases of large or recurrent uterine AVMs.
Medical therapy may be used to treat uterine AVM in women who want to preserve their fertility. This may include the use of hormonal therapy or antifibrinolytic agents.
The prognosis for women with uterine AVM is generally good. With appropriate treatment, most women will be able to control their bleeding and live normal lives. However, there is a small risk of recurrence, even after successful treatment.
Ultrasound images in this case are courtesy of Ms Regina Rachael.
For more information on this visit: