Ultrasound and Color Doppler Imaging Findings:
1. Left Upper Pole Large Parathyroid Adenoma:
- Ultrasound reveals a well-defined, hypoechoic mass measuring approximately [size] in the left upper pole of the neck, characteristic of a parathyroid adenoma.
- The adenoma may display a "halo sign," a hypoechoic rim surrounding the lesion, indicative of a capsule or fibrous tissue surrounding the adenoma.
- Color Doppler imaging may demonstrate peripheral vascularity within the lesion, suggestive of increased vascularity commonly seen in parathyroid adenomas.
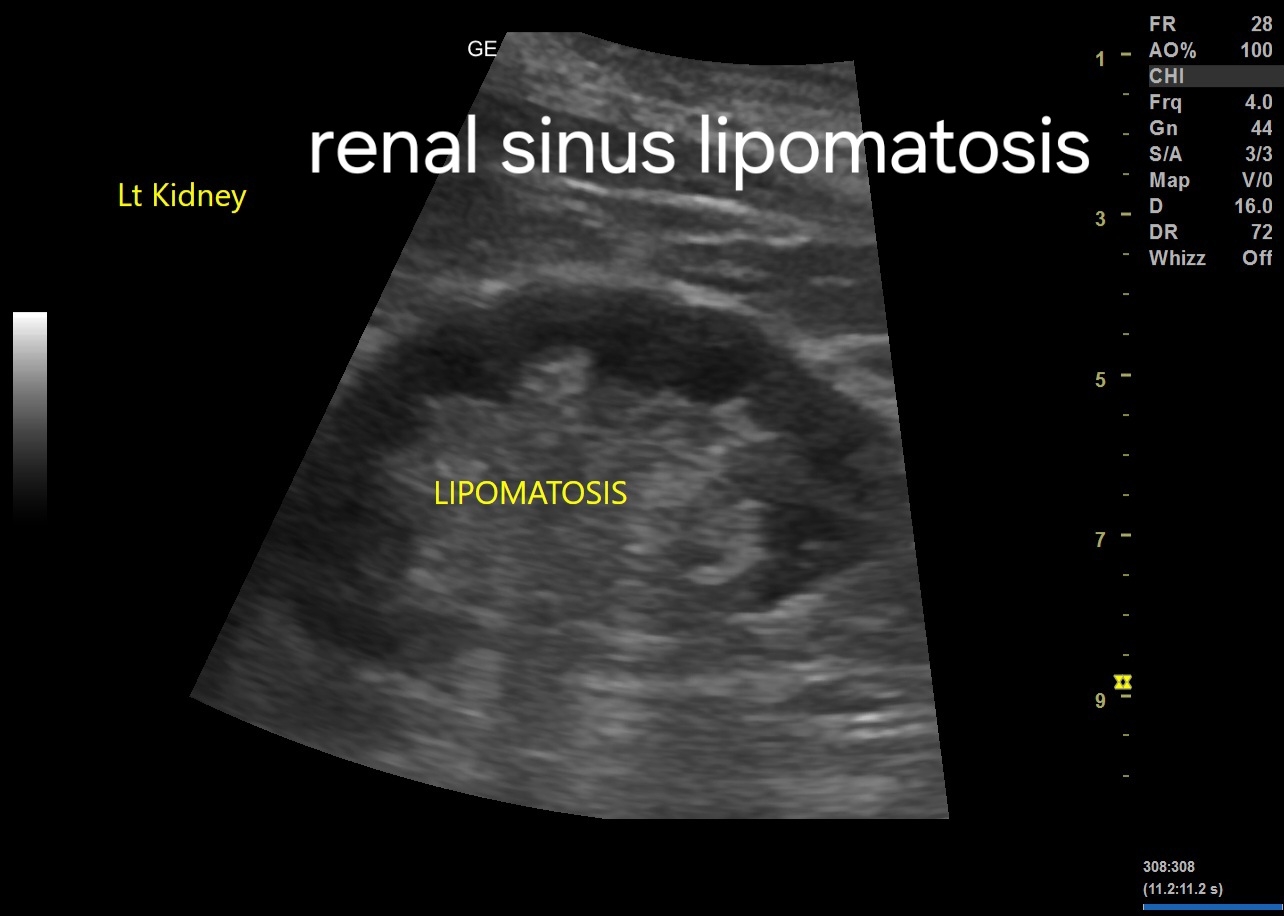
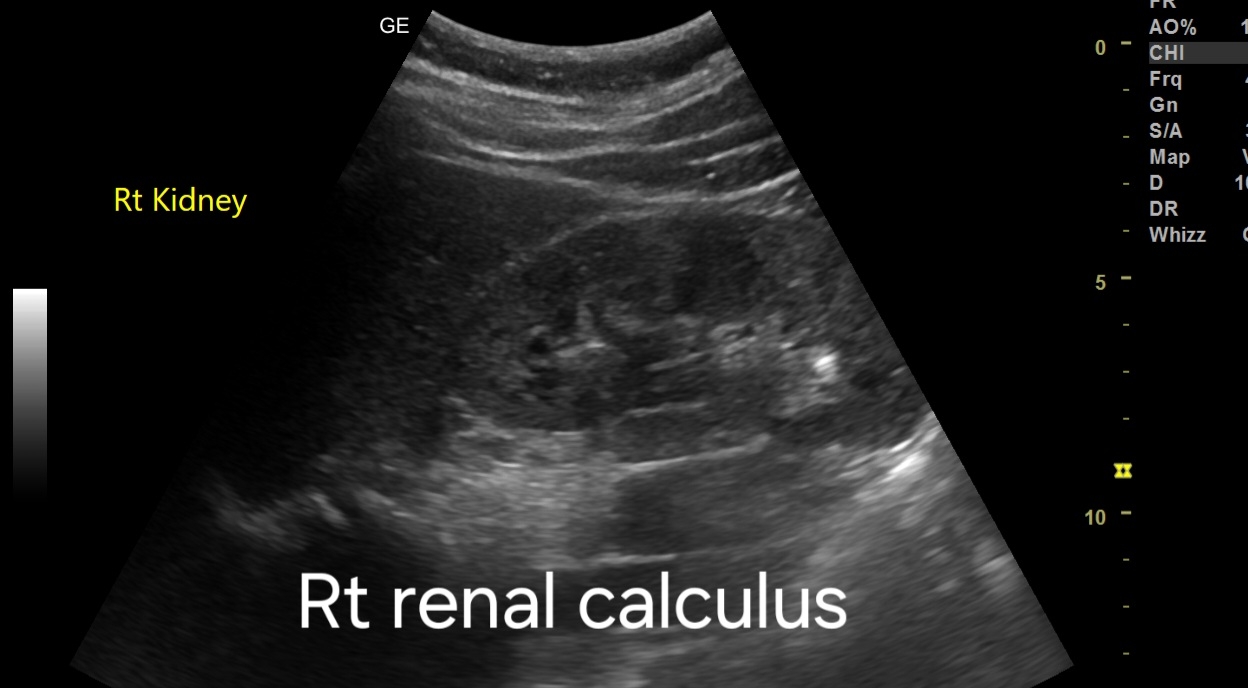
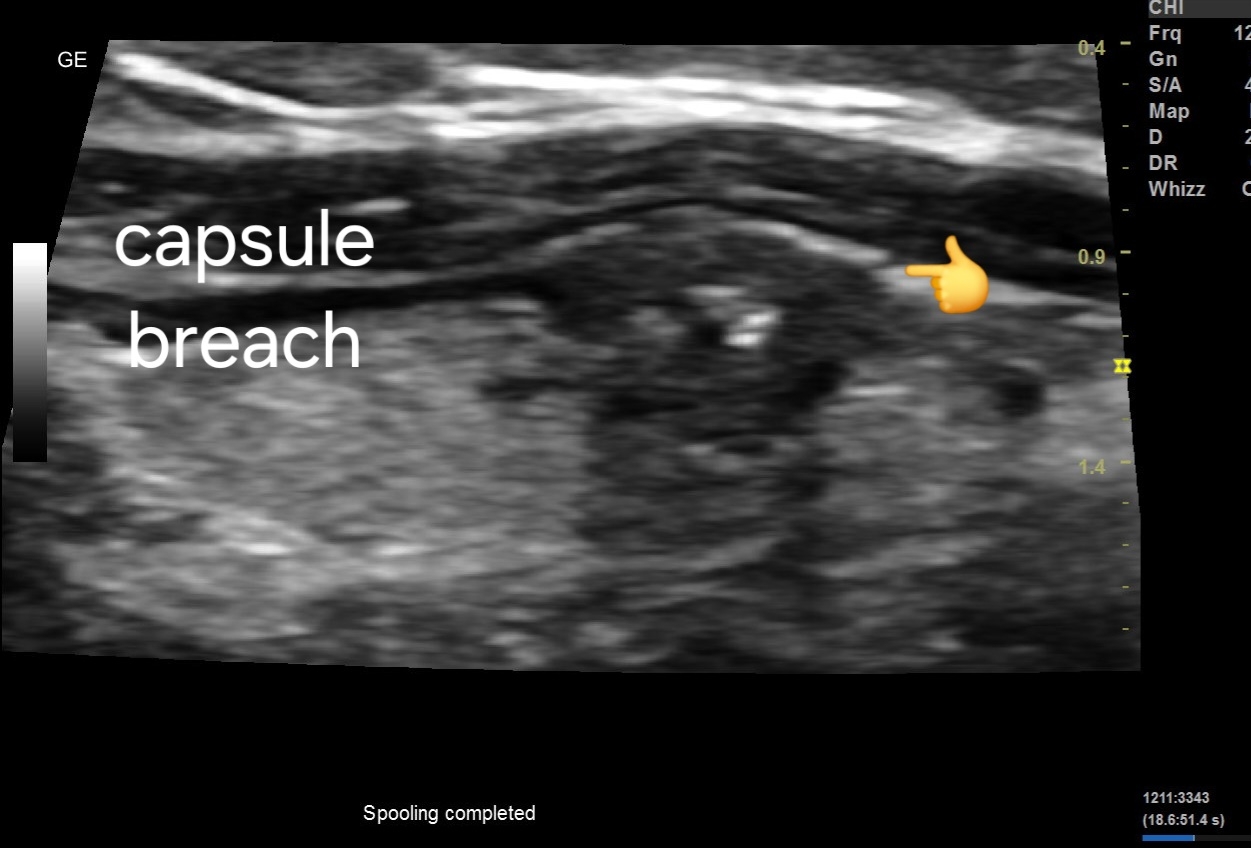
2. Small Renal Calculus:
- Ultrasound identifies a hyperechoic structure within the renal parenchyma measuring approximately [size], indicative of a small renal calculus.
- The calculus may cause posterior acoustic shadowing and may demonstrate twinkling artifacts on color Doppler imaging, aiding in its identification.
For more on this topic visit:
Further Radiological Investigations:
1. Parathyroid Adenoma:
- If ultrasound findings are inconclusive or additional characterization is required, further imaging modalities such as technetium-99m sestamibi scintigraphy or neck MRI may be indicated.
- Technetium-99m sestamibi scintigraphy is highly sensitive for localizing parathyroid adenomas, especially in cases of multiglandular disease or ectopic glands.
- Neck MRI provides detailed anatomical information and can help differentiate parathyroid adenomas from adjacent structures, aiding in surgical planning.
More about technetium-99m sestamibi scintigraphy:
Technetium-99m sestamibi scintigraphy is a nuclear medicine imaging technique used to localize parathyroid adenomas. Here's a brief description of the procedure:
1. Procedure:
- The patient is injected with technetium-99m sestamibi, a radiopharmaceutical agent that is preferentially taken up by parathyroid tissue due to its high mitochondrial content.
- After a period of uptake (usually 15-30 minutes), the patient undergoes imaging using a gamma camera.
2. Imaging Process:
- The gamma camera detects the emitted gamma rays from the technetium-99m sestamibi, producing images that highlight areas of increased radiotracer uptake.
- Parathyroid adenomas typically demonstrate increased uptake compared to surrounding tissues due to their higher metabolic activity.
3. Interpretation:
- Areas of increased radiotracer uptake on the images indicate the presence and location of parathyroid adenomas.
- The technique can distinguish between adenomas and normal or hyperplastic parathyroid tissue, aiding in surgical planning.
4. Advantages:
- Technetium-99m sestamibi scintigraphy is non-invasive and highly sensitive for detecting parathyroid adenomas, even in cases of ectopic glands or multiglandular disease.
- It provides functional information about parathyroid activity, complementing anatomical imaging modalities such as ultrasound or MRI.
5. Clinical Utility:
- The procedure is commonly used preoperatively to localize parathyroid adenomas in patients with primary hyperparathyroidism.
- It helps guide surgical intervention by identifying the exact location of the adenoma(s), facilitating targeted minimally invasive parathyroidectomy.
Overall, technetium-99m sestamibi scintigraphy is a valuable tool in the diagnostic workup and surgical management of parathyroid adenomas, providing functional localization information.
2. Renal Calculus:
- In cases where ultrasound findings are ambiguous or if further characterization is needed, a non-contrast CT scan of the abdomen and pelvis is recommended.
- CT scan provides superior visualization of renal calculi, allowing for accurate assessment of size, location, and composition.
- Dual-energy CT may be utilized to differentiate between types of renal calculi based on their composition, which can influence treatment decisions.
Also visit:
Prognosis and Management:
1. Prognosis:
- Prognosis for parathyroid adenomas is generally favorable with appropriate management.
- Early detection and intervention can prevent complications such as hypercalcemia and associated organ damage.
2. Management:
- Parathyroid Adenoma:
- Surgical excision is the mainstay of treatment for symptomatic adenomas or those causing significant hypercalcemia.
- Minimally invasive parathyroidectomy (MIP) using ultrasound or scintigraphy guidance is often preferred for localized adenomas.
- Long-term monitoring of serum calcium levels post-surgery is essential to assess for recurrence or persistent hyperparathyroidism.
- Renal Calculus:
- Treatment options include conservative management, extracorporeal shock wave lithotripsy (ESWL), ureteroscopy with laser lithotripsy, or percutaneous nephrolithotomy (PCNL) depending on the size and location of the stone.
- Adequate hydration and dietary modifications may aid in the prevention of recurrent stones.
- Follow-up imaging may be necessary to monitor for stone progression or recurrence.
*Note: Consultation with an endocrinologist and urologist is recommended for comprehensive management of the patient's conditions.