Painful menses, pelvic tenderness aggravated by menses.
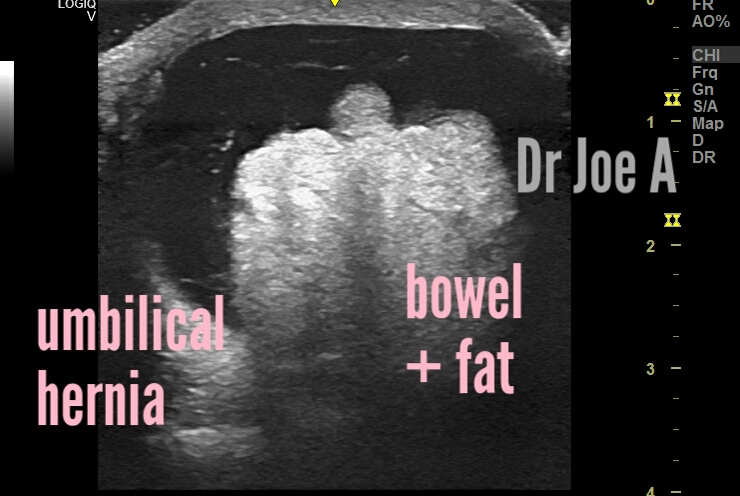
What does ultrasound reveal? Here are the ultrasound images:
Transabdominal sonography was sufficient we believe.
What are the findings?
Bulky, globular uterus.
Ultrasound findings in adenomyosis of the uterus:
Ultrasound findings in adenomyosis of the uterus:
Also:
Thickening of the uterine wall
Heterogeneous myometrial echotexture
Cystic or nodular areas within the myometrium
Poorly defined junctional zone
Presence of multiple small hypoechoic lesions within the myometrium
These ultrasound findings can aid in the diagnosis of adenomyosis, a common condition where endometrial tissue grows within the muscular walls of the uterus, causing painful and heavy periods.
Early detection and diagnosis of adenomyosis can help guide treatment options and improve quality of life for affected individuals.
What is the management of adenomyosis?
Management of adenomyosis includes several options that aim to alleviate symptoms and improve quality of life for those affected. Here are some common management strategies:
Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), hormonal contraceptives, and progestins can help manage pain and heavy bleeding.
Endometrial ablation or hysterectomy may be recommended for those with severe symptoms or who have completed childbearing.
Lifestyle changes such as maintaining a healthy weight, regular exercise, and stress management may also help alleviate symptoms.
Alternative therapies such as acupuncture and herbal remedies have shown promise in managing symptoms, although more research is needed.
A multidisciplinary approach involving gynecologists, pain specialists, and mental health professionals can also be beneficial in managing the physical and emotional aspects of adenomyosis.
For more visit: