*Initial Examination:
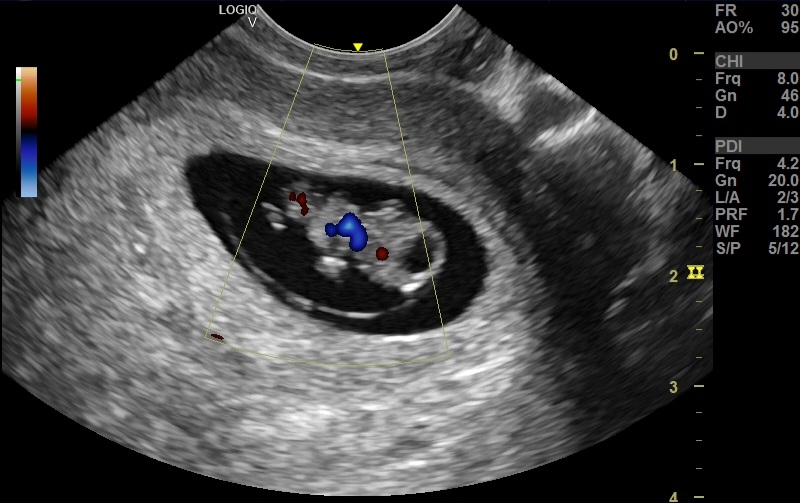
* Severe ascites: Fluid accumulation within the abdomen, indicative of advanced liver dysfunction.
* Moderate splenomegaly: Enlarged spleen, suggesting portal hypertension.
* Moderately advanced macro nodules: Regenerative nodules within the liver, typical of cirrhosis but at a potentially concerning size.
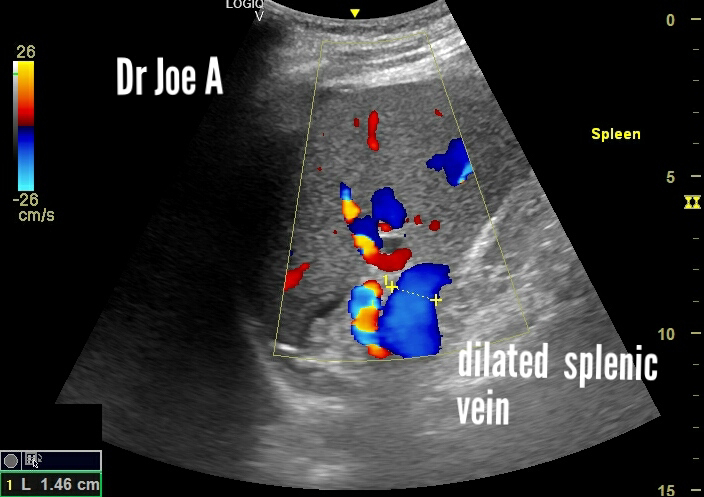
* Splenic vein:15 mm, exceeding normal diameter and further supporting portal hypertension.
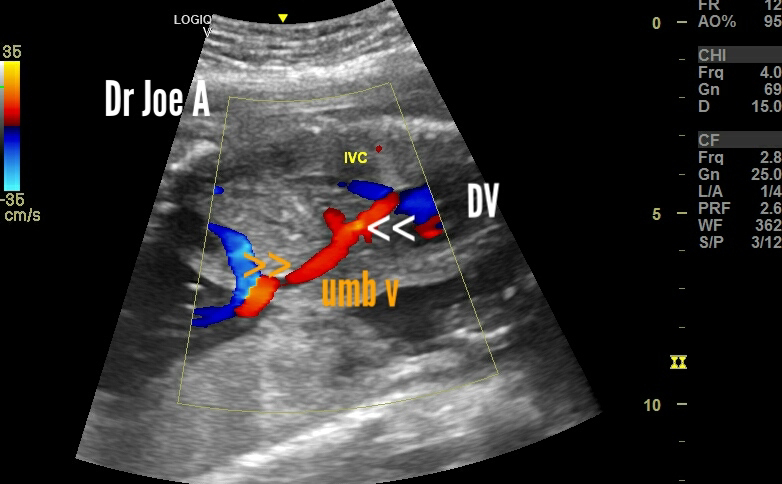
* Portal vein: 15 mm, also enlarged and consistent with portal hypertension.
*Follow-up Examination (after 1 year):
* Mild splenomegaly: Reduction in spleen size, indicating improvement in portal pressure.
* Splenic vein: Decreased in diameter, reflecting reduced portal congestion.
* Micronodular stage: Smaller regenerative nodules, suggesting regression of cirrhosis.
* Coarse echotexture: Persistent fibrous scarring within the liver parenchyma.
* No ascites: Absence of fluid collection, a major positive indicator.
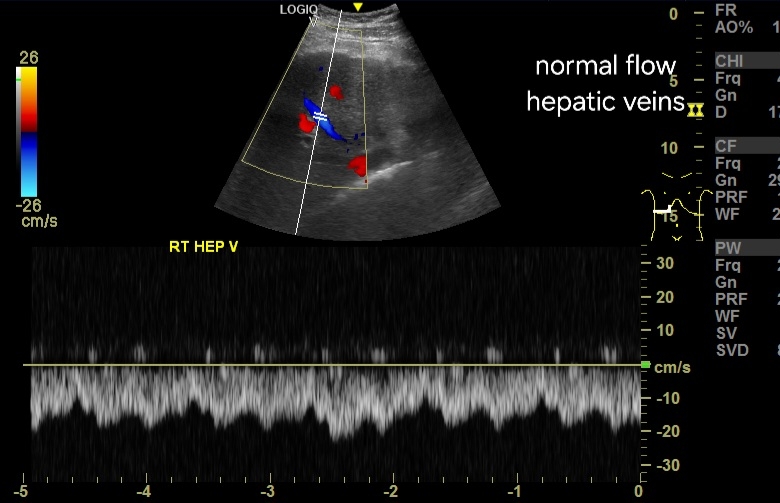
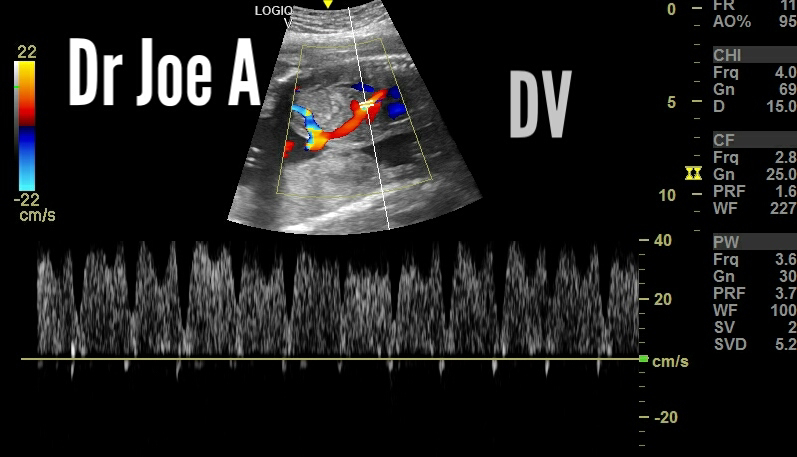
In both scans, portal vein and hepatic veins showed normal antegrade or forward flow suggestive of good prognosis.
* Overall:
* Marked improvement in ultrasound findings suggests effective treatment response for the patient's cirrhosis.
* Reduced size of spleen and splenic vein points to improved portal blood flow.
* Transition to micronodular stage signifies potential progress in reversing liver damage.
* Absence of ascites highlights significant clinical improvement.
For more information on this topic visit:
*Further Points to noe:
* Underlying cause of cirrhosis should be investigated for optimal disease management.
* Continued monitoring with ultrasound and other modalities is crucial to track disease progression and adjust treatment if needed.
*Note: This summary provides a general overview based on the information provided. For a complete and accurate assessment, consult the full medical records and consult with the patient's primary physician.