My latest ebook publication
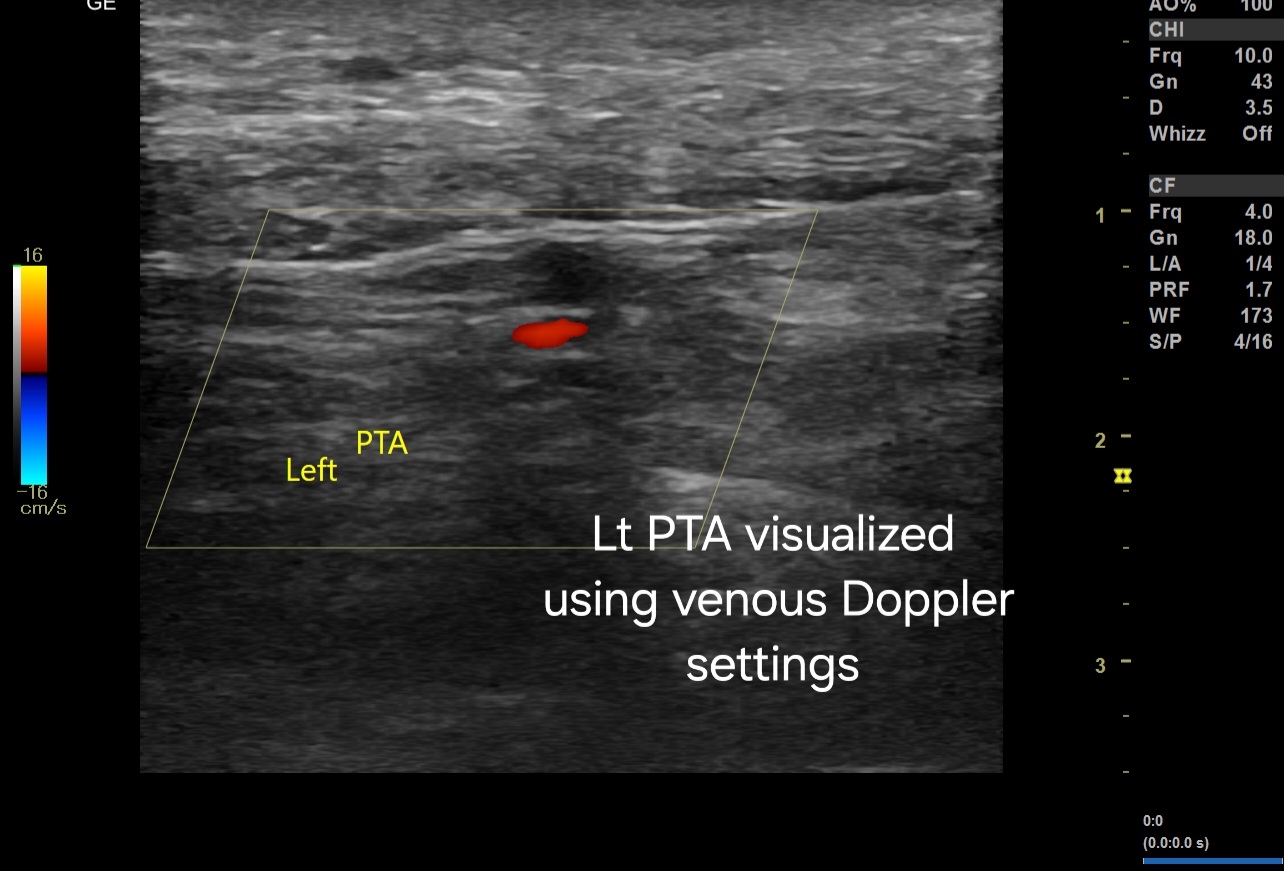
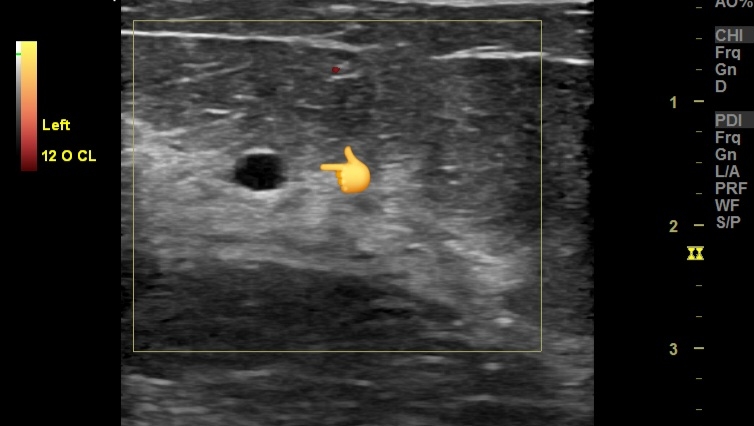
The "Ultrasound Atlas of the Urinary Tract" is a comprehensive 235-page ebook designed for radiologists and healthcare professionals. It features hundreds of high-resolution ultrasound images that meticulously cover the anatomy and pathology of the kidney, ureters, and urinary bladder. Utilizing B mode, color Doppler, and 3D ultrasound techniques, this atlas offers an in-depth visual reference for diagnostic imaging.
The book is structured to enhance understanding through detailed, annotated images, enabling precise identification of normal and abnormal findings. Each section systematically addresses the ultrasound appearances of various conditions, supported by a wealth of illustrative cases. Special attention is given to the applications of color Doppler and 3D ultrasound, showcasing their roles in providing additional diagnostic information and improving accuracy.
A dedicated chapter on renal Doppler enriches the content by delving into the vascular assessment of the kidneys. It covers key aspects such as renal artery stenosis, blood flow patterns, and hemodynamic changes, supported by clear, explanatory images.
Overall, this atlas serves as an invaluable resource for those involved in the diagnosis and management of urinary tract diseases, offering a blend of theoretical knowledge and practical insights through its extensive image library.
Available on Amazon Kindle app or reader 😊