#Etiology
- Traumatic Impact:
- Direct trauma to the chest, commonly seen in motor vehicle accidents.
- Blunt force impact leading to tissue injury and vessel disruption in the breasts.
#Pathology
- Seromas in the Breasts:
- Accumulation of serous fluid within a cavity formed by the disruption of breast tissues.
- Often forms in the subcutaneous or intermuscular spaces of the breast.
- Typically a result of surgical procedures or trauma.
- Hematomas in the Breasts:
- Collection of blood outside blood vessels, usually due to vessel rupture within the breast tissue.
- Can be located in the subcutaneous tissue, intermuscular planes, or deeper breast structures.
- Blood accumulation leads to varying stages of clot formation and organization.
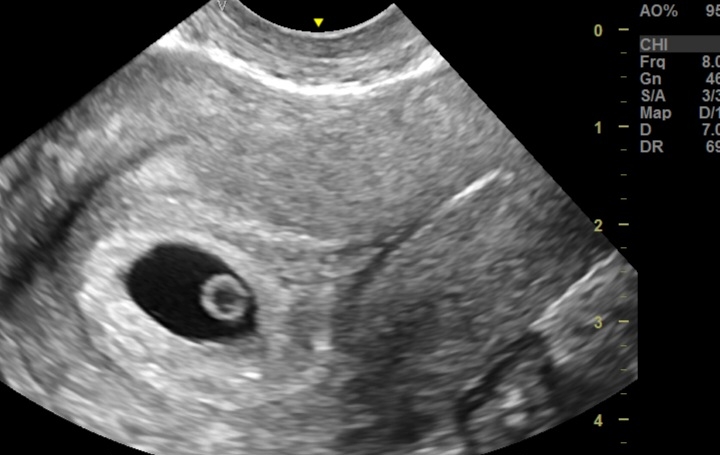
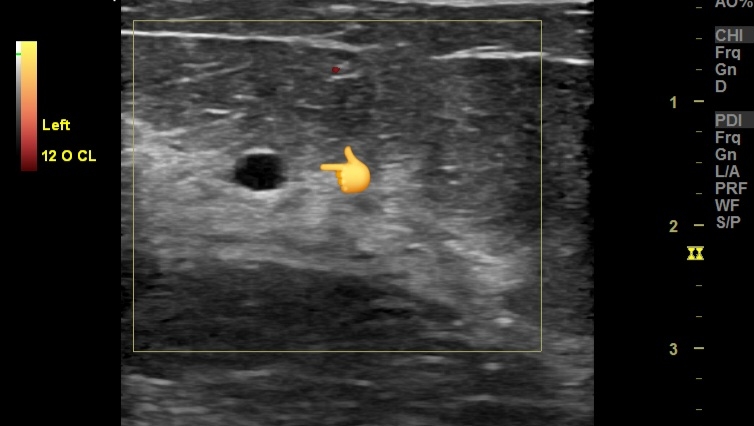
#Ultrasound Findings
- Seromas in the Breasts:
- Anechoic or hypoechoic fluid collections within the breast tissue.
- Well-defined margins.
- No internal vascularity.
- Posterior acoustic enhancement.
- Hematomas in the Breasts:
- Varying echogenicity depending on the age of the hematoma:
- Acute: Hyperechoic or mixed echogenicity.
- Subacute: Hypoechoic with internal echoes.
- Chronic: Anechoic or hypoechoic with a more organized appearance.
- Irregular or well-defined margins.
- Possible layering or fluid-fluid levels.
- No significant vascularity within the collection.
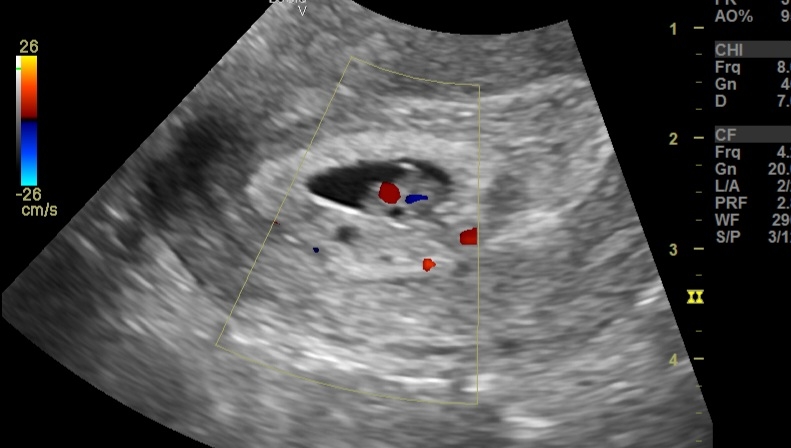
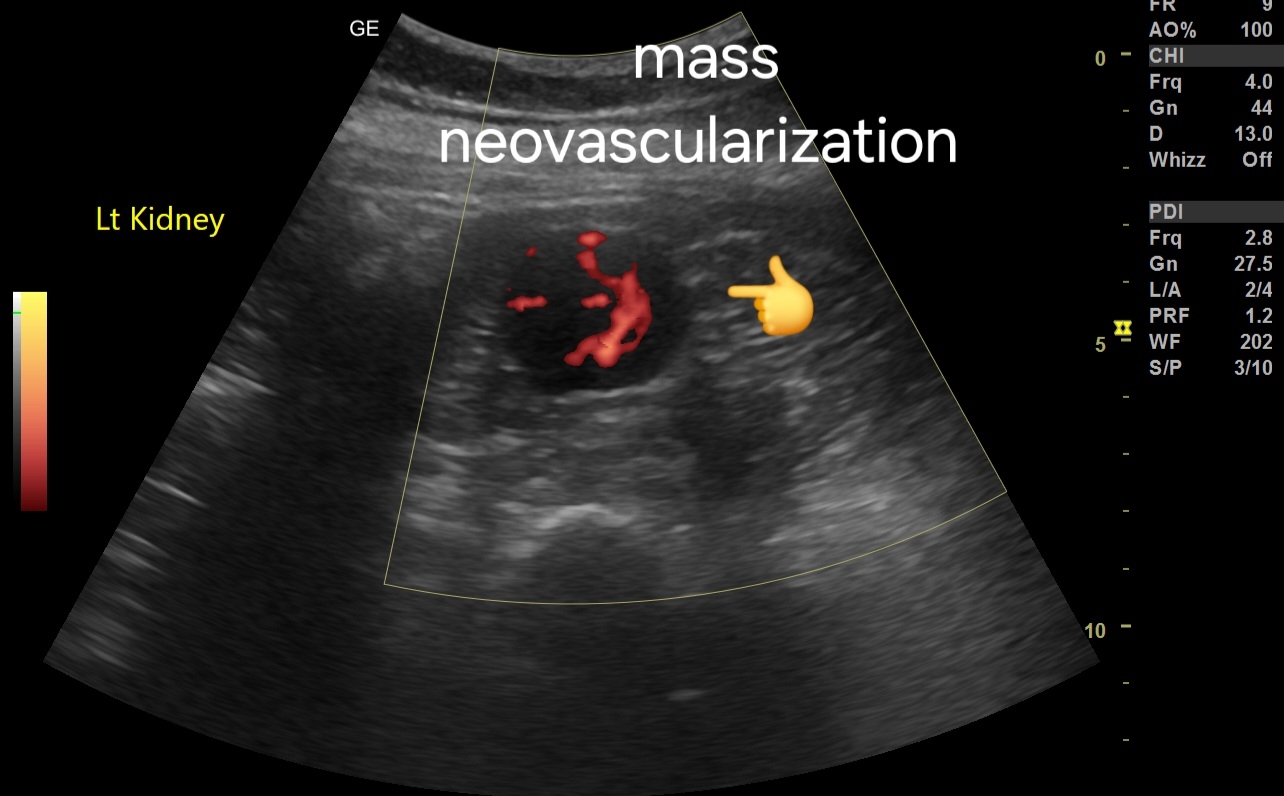
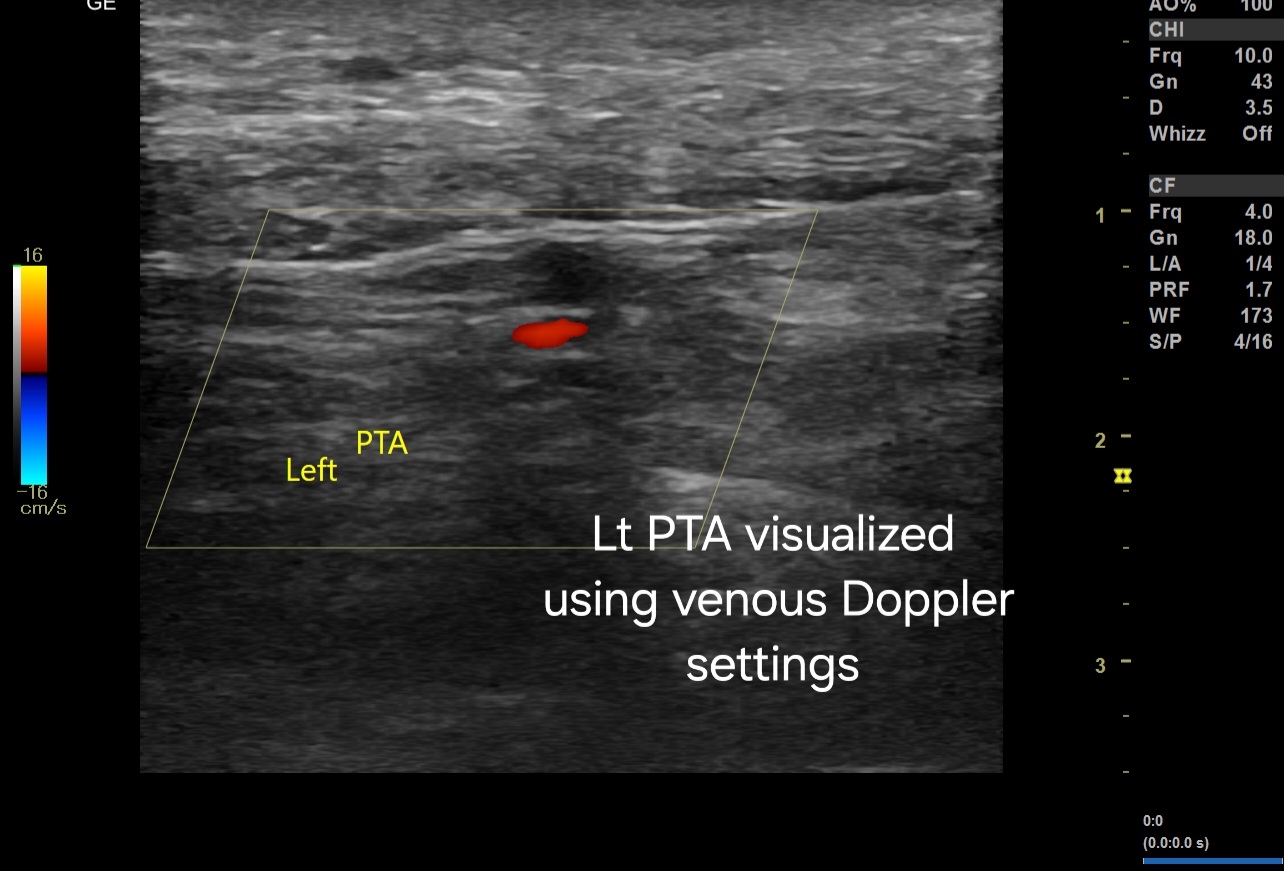
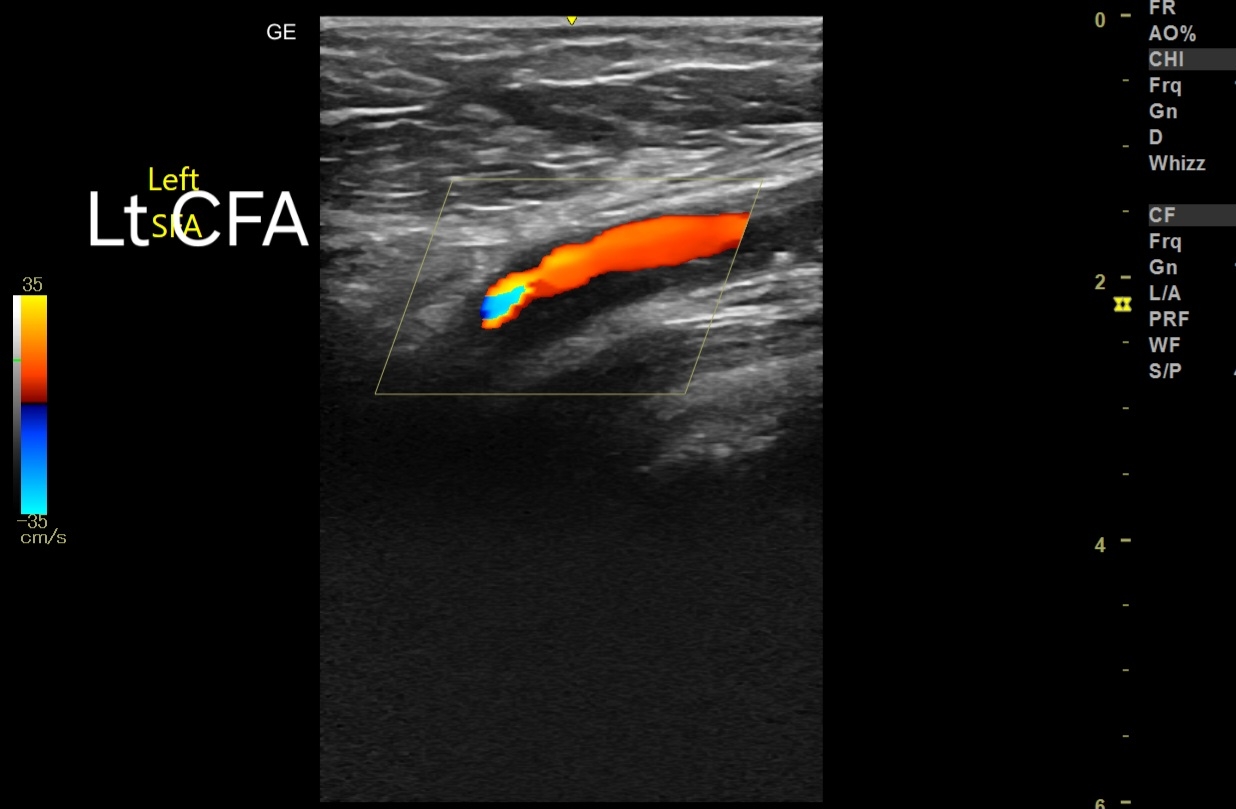
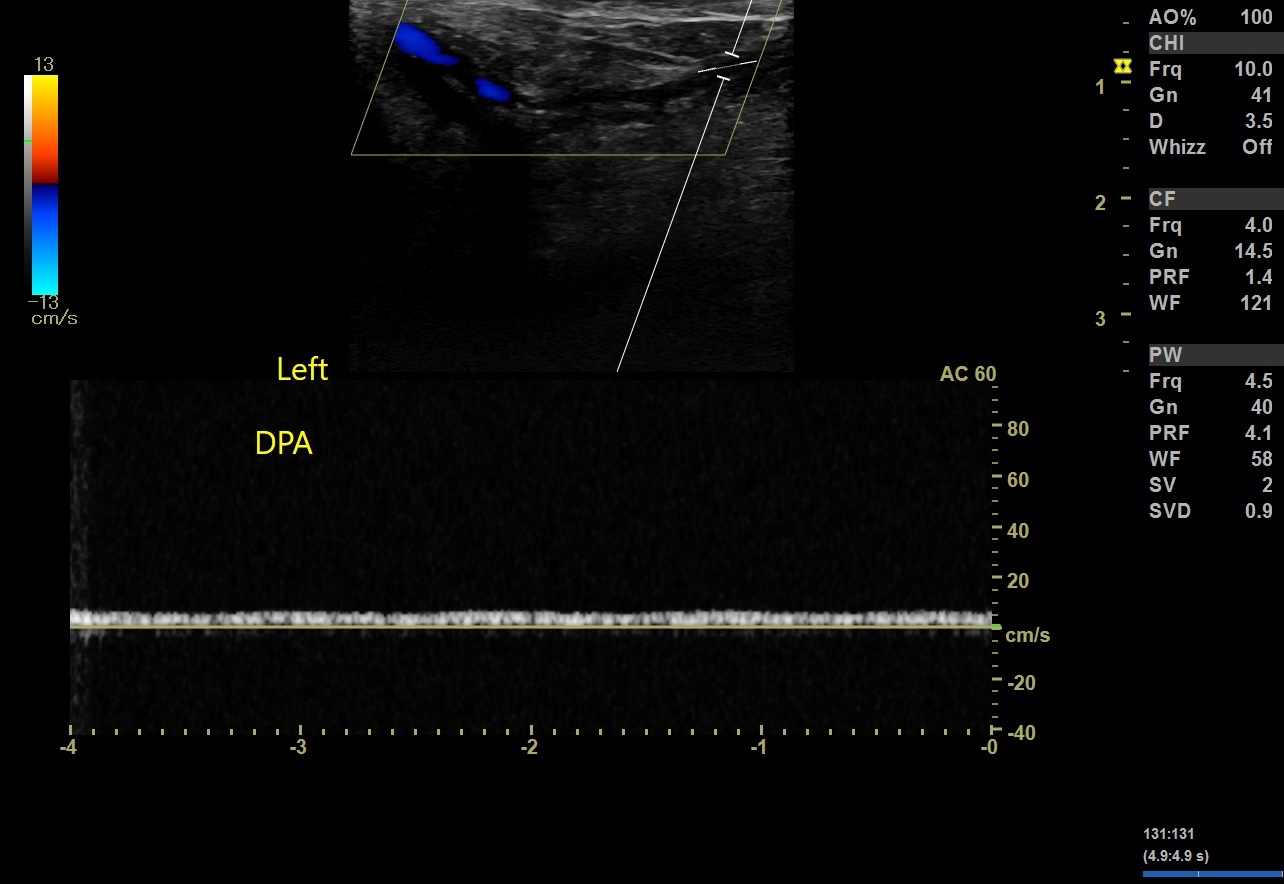
# Color Doppler Imaging Findings
- Seromas in the Breasts:
- No internal blood flow.
- Periphery might show slight increased vascularity due to inflammatory response.
- Hematomas in the Breasts:
- Typically, no internal vascularity.
- May see peripheral vascularity indicating the inflammatory response.
- In chronic cases, neovascularization around the hematoma capsule might be noted.
# Prognosis
- Generally favorable with appropriate management.
- Small, uncomplicated seromas and hematomas in the breasts often resolve spontaneously.
- Larger or symptomatic collections may require intervention.
# Management
- Conservative Treatment:
- Observation and follow-up with repeat imaging.
- Compression dressings.
- Analgesics and anti-inflammatory medications.
- Aspiration:
- Ultrasound-guided needle aspiration for large or symptomatic seromas in the breasts.
- Repeated aspiration may be necessary.
- Surgical Intervention:
- Drain placement for persistent or recurrent seromas in the breasts.
- Evacuation of hematoma if large, painful, or not resolving spontaneously.
- Surgical exploration in case of secondary infection or complications.
- Follow-Up:
- Regular clinical and imaging follow-up to monitor resolution.
- Monitoring for potential complications like infection or calcification in the breast tissue.
- Prevention of Recurrence:
- Adequate compression post-aspiration.
- Avoidance of trauma or excessive activity in the early recovery period.